Background:
Disseminated intravascular coagulation (DIC) is a severe, often fatal condition characterized by systemic coagulation activation leading to both widespread microvascular thrombosis and profuse hemorrhaging. Frequently associated with malignancies, DIC represents a serious clinical challenge. Lymphomas, characterized by their clinical diversity and varying prognoses, may present differing DIC risks across their subtypes.
Aim of the study
The study aims to understand how various lymphoma subtypes influence the development of DIC in hospitalized individuals, utilizing data from a national inpatient sample.
Methods and Materials
This study retrospectively examines a cohort of adult patients in the United States, hospitalized with DIC, both with and without lymphoma, utilizing the 2020 National Inpatient Sample (NIS). Patients were identified using the International Classification of Diseases (ICD-10) codes. Patients who were younger than age 18 years were excluded from the study. We used STATA for our analyses. Fisher's exact test was utilized for comparing proportions, while Student's t-test was employed for the comparison of continuous variables. We performed a multivariate logistic regression analysis, taking into consideration various patient, and hospital characteristics including age, gender, race, median zip income, insurance status, hospital geographical region and location, bed size, urban or rural setting, teaching status to identify the adjusted odds ratio for the development of DIC in different lymphoma subtypes. The Charlson comorbidity index was utilized to account for the burden of comorbidities in the analysis.
Results
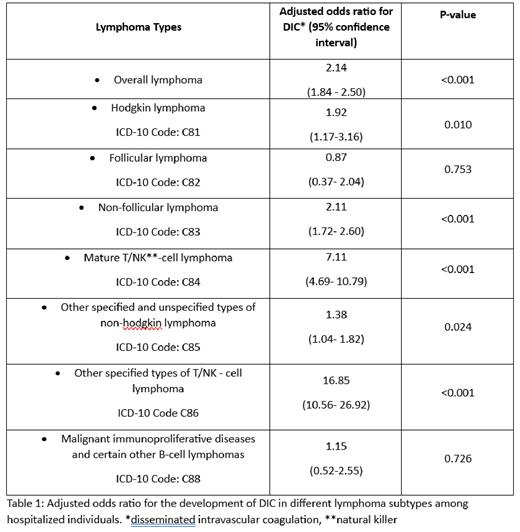
Among 48,310 adult DIC patients in the 2020 NIS dataset, 2.48% concurrently had lymphoma. A significant disparity was noted in gender distribution, with fewer females in the lymphoma group (40% vs 49%, p=0.0135). Patients with lymphoma were, on average, older with a mean age of 62.72 years. The racial composition between the two groups was not significantly different (p=0.651). The odds of developing DIC were significantly increased overall in lymphoma patients (aOR=2.14, p <0.001). Of the lymphoma subtypes, other specified types of T/NK- cell lymphoma (natural killer) (grouped under the ICD-10 code: C86, and further sub-categorized into extra-nodal NK/T cell lymphoma, hepatosplenic, intestinal, subcutaneous, angioimmunoblastic, primary cutaneous T cell lymphoma, and blastic NK-cell lymphoma) exhibited the highest risk of DIC development (aOR=16.85, p <0.001).
Non-follicular, mature T-NK-cell, other specified and unspecified types of Non-Hodgkin, and Hodgkin lymphomas also showed significant DIC risks (p<0.05), whereas no statistically significant risks were found in follicular lymphoma (p=0.753) and malignant immunoproliferative diseases and certain other B-cell lymphomas (p=0.726). See Table 1 for further details.
Conclusion:
This study underlines a significant association between lymphoma and elevated risk of DIC, with the highest odds observed in other specified types of T/NK- cell lymphoma. Clinical diversity within lymphoma subtypes influenced DIC risks differently, underlining the importance of individualized care. In clinical practice, increased vigilance for DIC is suggested in lymphoma patients. Prompt identification and management of DIC in this patient population could potentially improve outcomes in healthcare optimization. Further studies are warranted to elucidate the underlying mechanisms and to explore potential targeted interventions.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal